Updated: January 25, 2022
Introduction:
This resource outlines the benefits of Collaborative Care and is designed to be shared with PCPs, stakeholders, and others looking to implement CoCM.
For a printable version, download the resource below. A printable PDF is available for download; however, please note that this document may not conform to the WCAG-2 accessibility standards.
Why Practice Collaborative Care?
Collaborative care (CoCM) is beneficial to primary care providers (PCPs) and their patients because it offers better
medical care, access to psychiatry experts, helps with challenging patient cases, and team collaboration.

Established Evidence Base
- CoCM has a robust evidence base of over 80 randomized controlled trials and has been shown to be the best approach to treating depression in many populations and settings.
- CoCM has a strong and expanding evidence base for its use with diverse behavioral health diagnoses such as anxiety, posttraumatic stress disorder, chronic pain, and dementia.

Better Medical Outcomes
- CoCM is linked to better medical outcomes for patients with diabetes, cardiovascular disease, cancer, and chronic arthritis.
- CoCM is recommended as a primary prevention strategy for cardiovascular events in patients without preexisting heart disease (Psychosomatic Medicine, 2014).

Help with Challenging Patient Cases
- Many challenging cases likely have patients with untreated or undertreated behavioral health conditions. Behavioral health providers do the follow-up and intervention tasks that a busy PCP doesn’t have time to do, but make a big difference for patients.
- PCPs are generally more satisfied working within an integrated behavioral health care program than within usual care (Family Community Health, 2015).

Faster Improvement
- A 2016 retrospective study at Mayo Clinic found that the time to depression remission was 86 days in a CoCM program while in usual care it was 614 days.
- Analysis of a large CoCM implementation found that early, intense intervention by the behavioral health provider was key to early improvement in patients with depression symptoms (Psychiatric Services, 2015).
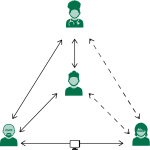
It Takes a Team
- CoCM uses an enhanced care team to provide a population based, treat-to-target approach to care. Through shared care planning, the team makes proactive changes in treatment to make sure that no patients fall through the cracks.
- Only 30-50% of patients have a full response to the first treatment. That means 50-70% of patients need at least one treatment adjustment. Additional experts can help.