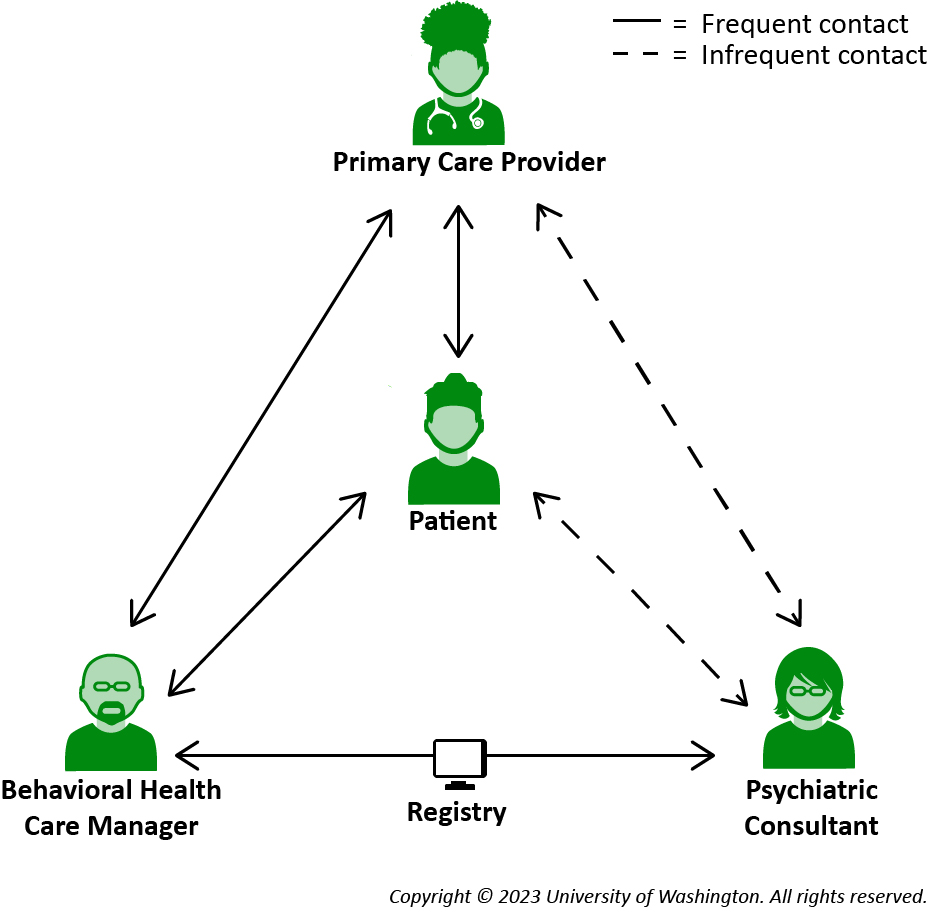
This guide describes the features of a registry to support Collaborative Care (CoCM) workflows. The descriptions can help you evaluate whether a registry will meet the needs of your program, or as a starting point for building your own tool.
CoCM registries vary widely in their sophistication, functionality, cost, and scalability. Options include:
- A spreadsheet used alongside the EHR
- The AIMS Caseload Tracker
- A custom registry within the EHR or care management software system
One registry option is the AIMS Caseload Tracker, designed by the AIMS Center for behavioral health teams working in integrated care settings.