For 20 years, the AIMS Center has supported diverse healthcare organizations in integrating behavioral health services into medical settings. We’ve learned some things along the way! To celebrate our 20th Anniversary, we will share our insights throughout 2024 in monthly “Lessons Learned.”

Miss a lesson? Find the archive below.
To receive lessons directly in your inbox, sign up for AIMS Center Updates.

Quick Read
-
- Primary Care Providers (PCP) are central to Collaborative Care (CoCM).
-
- To run a successful CoCM program you need buy-in and active participation from your PCPs.
-
- PCPs benefit from training and tools designed to aid them in their CoCM role.
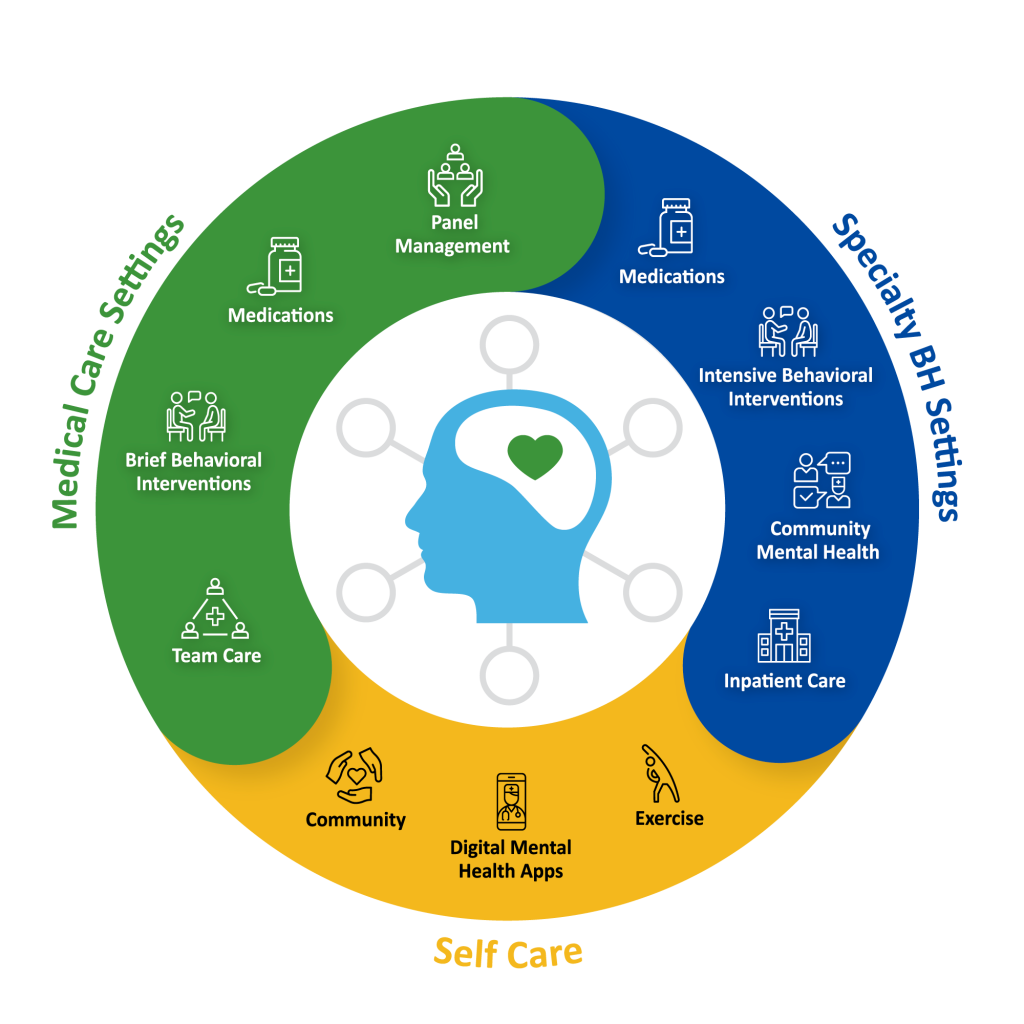
It is impossible to overstate the importance of the Primary Care Provider (PCP) in Collaborative Care (CoCM). There is a reason why they are at the apex of the care triangle (graphic above). CoCM often starts with the relationship between the patient and the PCP. Additionally, the PCP directs the care delivered by the CoCM team. When building the CoCM treatment team, implementing organizations often expend substantial time, money, and energy hiring the Behavioral Health Care Manager and Psychiatric Consultant. While this is important, organizations should ensure the PCP is a primary partner in CoCM implementation. When the PCP is an afterthought we sometimes see in implementations that struggle.
LINCHPIN FOR SUCCESSFUL COCM IMPLEMENTATION
When patients are identified through screening, the PCP is often best positioned to connect the patient to CoCM. They are typically the one who talks with the patient about the symptoms they are experiencing and the treatment the clinic offers. Additionally, when the clinic is billing the CoCM codes, the PCP is also the person who obtains verbal consent from the patient (except in FQHCs and RHCs where clinical staff can serve in that role).
A robust endorsement from the PCP is a powerful engagement tool. Most patients care what their provider thinks, and a strong recommendation to participate in Collaborative Care can set the care journey off on the right path. To do this well, the PCP needs an informative and engaging ‘elevator pitch’ about CoCM to use with patients.
SUPPORTING PCPS IN COCM
Collaborative Care is not a referral model. The PCP remains an active member of the treatment team, prescribing medications when that is part of the treatment plan. Sometimes PCPs feel underprepared to play that role and don’t understand why the psychiatric provider doesn’t just take over the patient’s care. Or they may feel like they have everything under control and don’t need support from the psychiatric provider, but 20 years of research has shown that patients receiving treatment from their PCP alone are half as likely to improve.
As a key partner in building successful CoCM, PCPs benefit from orientation and preparation for their vital role. The AIMS Center provides tools and materials designed to support PCPs, including free training developed in partnership with the American Psychiatric Association.

Quick Read
- Historically marginalized communities can have limited access to behavioral health treatment and can experience less robust clinical outcomes because of poorer quality care.
- Research shows Collaborative Care (CoCM) improves behavioral health outcomes for patients from racial and ethnic minority groups.
- CoCM reduces health disparities by expanding access to evidence-based behavioral health care and offering non-medication treatment options.
Although the prevalence of mental health conditions is equivalent between racial/ethnic groups, treatment access and clinical outcomes can be significantly worse for people from historically marginalized communities. They are less likely to access mental health services and, when they do access care, are more likely to receive lower quality of care and to have poorer outcomes. Collaborative Care (CoCM) can reverse that.
What Research Shows
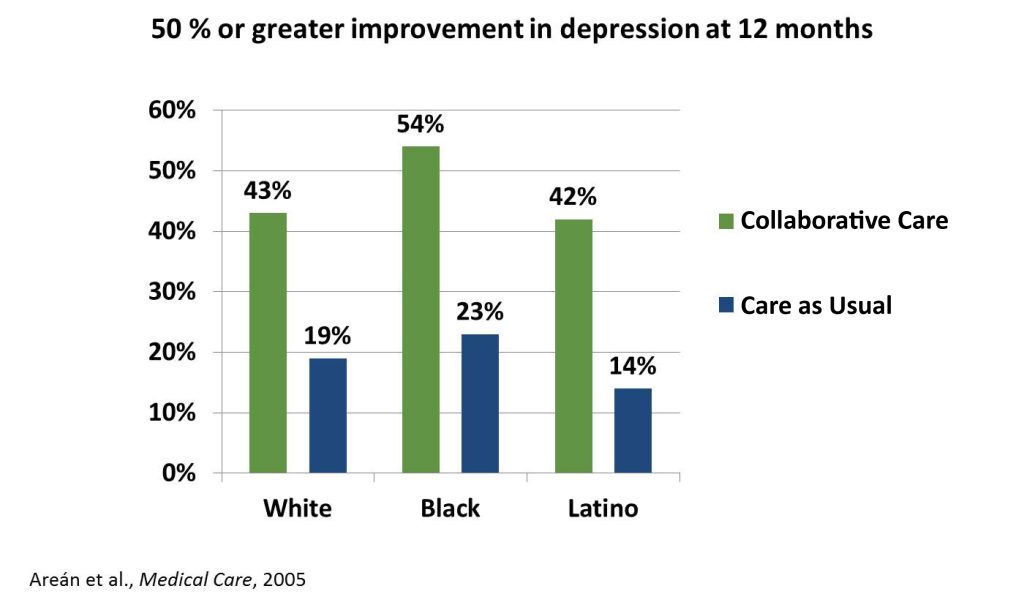
A landmark study in 2005 compared clinical outcomes between White, Black and/or African American, and Latinx patients receiving either usual depression treatment or Collaborative Care (CoCM).1 As the graph below shows, all patients were significantly more likely to have a 50% or greater improvement in depression symptoms when treated with CoCM as compared with usual depression treatment. The relative benefit of CoCM was highest for patients who were Black and/or African American (31% greater likelihood of depression improvement) and Latinx (28% greater likelihood) than for White patients (24% greater likelihood), though this difference was not statistically significant.
A systematic review of 19 studies published in 20202 included ten randomized controlled trials (the highest quality of research evidence) and nine observational studies. All of the studies included the five core principles of CoCM. One of the challenges they encountered is that there is no standard definition of culturally sensitive care. Despite this, these studies demonstrated that CoCM – even without cultural or linguistic tailoring – was effective at improving depression outcomes for Black and/or African American, Latinx, Asian, and American Indian or Alaska Native patients, including those from low socioeconomic backgrounds.
How Collaborative Care Reduces Disparities
Patients from racial and ethnic minority groups often experience entrenched and systemic health disparities. Collaborative Care (CoCM) works to reduce these disparities by:
-
- Increasing access to care in a less stigmatizing environment than traditional specialty behavioral health settings.
- Offering non-medication treatments. Research has shown that patients from racial/ethnic minority groups have a stronger preference for non-medication treatments. One of the things that differentiates CoCM from usual care is the addition of behavioral treatments offered in the medical setting.
- CoCM increases access to evidence-based behavioral health care, something that is not available to all patients equitably.
To learn more and to read the studies behind the headlines, visit our evidence-base page and select “Treating Racial and Ethnic Groups with CoCM.”
1. Arean P, et. al. Improving depression care for older, minority patients in primary care. Medical Care, Apr 2005; 43(4):381-390.
2. Hu J, et. al. The effectiveness of Collaborative Care on depression outcomes for racial/ethnic minority populations in primary care: A systematic review. Psychosomatics. Nov-Dec 2020; 61(6):632-644.

QUICK READ
- Successful Collaborative Care programs include a well-run, weekly Systematic Caseload Review meeting between the Behavioral Health Care Manager and the Psychiatric Consultant.
- The Systematic Caseload Review allows the Psychiatric Consultant to oversee treatment progress and make proactive changes to the treatment plan.
- A set weekly meeting ensures high-quality patient care, resulting in more people receiving care and their symptoms improving faster.
Over the past 20 years, we have seen that if the Systematic Caseload Review (SCR) is not functioning optimally, it will undermine the effectiveness of your entire Collaborative Care (CoCM) program. The SCR sets CoCM apart from other integrated care approaches. In this weekly meeting, the Behavioral Health Care Manager (BHCM) and the Psychiatric Consultant have dedicated time to examine a registry and identify which patients need an individual case review that week.
Within the SCR, the Psychiatric Consultant can assist with diagnostically complex patients and make treatment suggestions based on information they receive from the registry, the electronic health record (EHR), and the BHCM. This structure allows the team to leverage limited Psychiatric Consultant expertise as, typically, the Psychiatric Consultant does not see patients directly.
What Collaborative Care Experts Know
It is not enough to schedule time between the Psychiatric Consultant and the BHCM and assume everything will go well. An article by Bauer and colleagues articulates the vital features of an effective SCR and the threats to success and their solutions. These are some of the main points that align with our experience:
- Regularity and duration: Meetings should occur weekly, even if the program is new and caseloads are small. It is essential for this not to be an ad hoc meeting or a 'call me when you have questions' scenario. The length of the meeting should match the number and complexity of patients. If the BHCM has a caseload above 75 patients, the SCR may need longer than an hour. Similarly, if there is more than one BHCM in the SCR meeting, the length should increase commensurately.
- Set an agenda and come prepared: An effective SCR has a focused agenda that enables the team to review six to ten patients each hour. Before the meeting, the BHCM and Psychiatric Consultant should create an agenda and review the registry to prepare for the SCR. One of the biggest mistakes we see is that the Psychiatric Consultant does not have an equal role in preparing for the SCR and setting the agenda. Having a second set of eyes on the registry is critically important to identify patients who are not improving quickly enough or those who are ready for relapse prevention planning and ending their episode of care.
- Action items and follow-through: A good Systematic Caseload Review generates action items. The BHCM and the Psychiatric Consultant must clearly articulate each action item and who is responsible for follow-through. It is a best practice for the Psychiatric Consultant to make their treatment recommendations directly to the Primary Care Provider (PCP) through the EHR, as this creates a communication channel for the PCP to ask questions about the recommendations. Before each SCR, the BHCM should check the EHR to determine if recommendations from last week's SCR have been implemented. If not, the BHCM and Psychiatric Consultant should discuss an action plan for follow-up with the PCP.
- Behavioral Health Care Manager support: A good SCR is about more than treatment recommendations - it's an opportunity for the Psychiatric Consultant to support the BHCM. In their clinic, the BHCM may be the only person in their role or the only behavioral health provider. They benefit from having an opportunity to talk with the Psychiatric Consultant about the challenges they face and receive support and advice. It is also an opportunity for the Psychiatric Consultant to teach the BHCM about medications, differential diagnosis, and other topics that will help them work together more successfully.
The Systematic Caseload Review offers an efficient and cost-effective method of bringing specialist-driven care into the primary care setting. Ensuring a defined population of patients can receive care informed by a Psychiatric Consultant, usually allowing the Psychiatric Consultant to treat more patients than they could directly. A well-functioning Systematic Caseload Review will set your Collaborative Care program up for success.

Quick Read
- Just as you measure outcomes with your patients, it is essential to measure outcomes of your Collaborative Care program.
- Performance metrics can be mapped onto the core principles for Collaborative Care.
- Your team should meet regularly to review metrics and use a continuous quality improvement approach to improve your program.
Effective Collaborative Care (CoCM) programs utilize metrics to track their progress and results. Regularly measuring your program’s performance allows you to diagnose implementation challenges and intervene before they become entrenched and undermine your success. You can monitor a variety of metrics that correspond to the core principles of CoCM.
 Patient-Centered
Patient-Centered
Measuring patient satisfaction allows CoCM programs to hear directly from their patients. Patient feedback is powerful. In the landmark IMPACT research trial, patients receiving CoCM were significantly more satisfied with their care than patients receiving usual care. Your team can identify strategies to collect this vital feedback.
 Population-Based
Population-Based
It is crucial to understand the reach of your program. Standard areas of focus include:
-
-
-
-
- Does your screening workflow have adequate reach and match the patient population you want to serve with CoCM?
- Is the average time between identification and the first visit with the Behavioral Health Care Manager (BHCM) under two weeks?
- Is the referral rate of new patients adequate to build and sustain the program?
- Do patients who are referred enroll?
- Are patients being seen more than once per month on average?
- Are patients out of contact for over two months being deactivated from the caseload to make room for new patients?
-
-
-
![]()
Measurement-Based Treatment to Target
Most CoCM programs monitor patient clinical outcomes – improvement, response, remission – and compare their outcome rates to published standards. If your program is not getting as many people better as expected, you can dig into potential reasons. Are symptoms being remeasured frequently enough to be able to see improvement? Are you reaching 6-10 patients per 1.0 FTE BHCM with the weekly Systematic Caseload Review (SCR)? Are patients not improving quickly enough prioritized for discussion during the SCR?
![]()
Evidence-based Treatments
Your team needs to consider the common conditions targeted by your CoCM program. Are patients offered the full range of evidence-based treatments, including medications and behavioral treatments? Are evidence-based psychotherapies being used?
![]()
Accountable
At the core of this principle is the process of monitoring metrics and adjusting care delivery as needed. Do the processes of care and clinical outcomes align with your organization’s vision, goals, and expectations?
Once you have selected a set of metrics, your team should meet regularly, at least quarterly, to review them with clinical and organizational leadership. If you are not achieving your goals, investigate potential causes and use a continuous quality improvement approach to try interventions to improve them. If you are hitting your targets, perhaps it’s time to stretch beyond where you are now by setting them a bit higher or identifying new impact areas to monitor.

Quick Read
- There is robust research on the effectiveness of Collaborative Care in specialty medical settings.
- Patients facing complex medical diagnoses also experience a heightened depression risk and Collaborative Care significantly improves their outcomes.
- Successful implementation of Collaborative Care in specialty medical settings requires deliberate strategy and thoughtful execution.
Collaborative Care (CoCM) often brings to mind primary care settings, but its benefits extend far beyond. Specialty medical settings have been using CoCM for years to address the complex needs of patients with various comorbid medical conditions. Implementing a successful CoCM program in this context requires careful consideration and planning. Yet, the substantial improvement in patient health outcomes justifies the effort.
Collaborative Care's Impact on...
Patients with Diabetes
According to the Centers for Disease Control and Prevention, individuals with diabetes face a higher risk of depression compared to the general population. For those with Type 1 Diabetes, this risk doubles, and with Type 2, it triples. The reciprocal relationship between diabetes and depression (depression can exacerbate diabetes, and vice versa) complicates patient care. Over the past two decades research examining the effects of CoCM on depression and diabetes outcomes, reveals that when patients receive CoCM focused solely on depression they have a significant improvement in depression but no improvement in glycemic control/HbA1c values. However, when the CoCM approach addressed depression and diabetes, patients showed improvement in both areas.
Patients with Heart Disease
A quarter of patients battling heart disease experience depression - a rate that is more than double that of those without cardiovascular conditions. Similar to diabetes, there's a reciprocal relationship between heart disease and depression, where one condition can worsen the other. Most studies of CoCM for patients with cardiovascular disease have shown a significant improvement in mood and quality of life. However, differences have not been observed in rates of hospitalization or mortality.
Patients with Cancer
Up to 25% of patients with cancer experience depression, which can negatively affect the quality of life and the ability to engage effectively in cancer treatment. When treated with CoCM as compared to usual care, patients with cancer and depression experienced decreases in depressive symptoms, pain, and fatigue.
Implementation Considerations
Implementing CoCM in specialty medical settings requires thoughtful consideration of the differences between primary and specialty care. For example, a common issue that arises is who will prescribe psychiatric medications when they are part of the treatment plan. Many specialists may hesitate to take on the role of primary prescriber for psychotropic medications. To manage this challenge, some organizations offer the specialty provider extra support from the Psychiatric Consultant, who takes on that role, sometimes including a one-time psychiatric evaluation and closer communication about medication initiation and changes.
When the healthcare organization provides both primary and specialty care to the patient, they can coordinate prescribing with the Primary Care Provider. Other aspects of CoCM, including the contributions of the Behavioral Health Care Manager and the Psychiatric Consultant, are provided in collaboration with the specialty care CoCM team.
While it takes some extra thought to implement CoCM in specialty medical settings, it can be successful. The benefits for the patient's quality of life, mental health symptoms, and physical health symptoms make it worth the effort.

Quick Read
- Since its inception, CoCM has evolved significantly and the evidence base shows it is significantly more effective than usual care in treating a variety of behavioral health conditions.
- Providing CoCM for diverse conditions sometimes requires an adjustment to how the model is delivered.
- It is important to consider which health conditions your CoCM program will address and tailor your hiring and training to meet these specific health needs.
Initial studies on the Collaborative Care Model (CoCM) were primarily centered around depression, the foremost cause of disability globally. Once a solid evidence base was built for the effectiveness of CoCM in managing depression, the scope of research broadened to include anxiety disorders. With the oldest and most robust research on CoCM examining depression and anxiety, some have the misconception that the efficacy of CoCM is limited to just these conditions, but that is not the case.
Over the past 20 years, researchers have studied the effectiveness of CoCM for diverse conditions, and it has proven to be significantly more effective than usual care for several other conditions. However, it’s important to note that achieving these outcomes sometimes necessitates modifications in how the model is delivered.
The Impact of CoCM on Various Conditions
Post-traumatic Stress Disorder (PTSD)
There is now a significant evidence base supporting CoCM as an effective treatment for PTSD. Much of this work has occurred in the Veterans Administration (VA) healthcare delivery system (such as this 2015 study examining telehealth for PTSD). Studies from outside the VA have further demonstrated its effectiveness. For instance, this study found that the use of CoCM for people hospitalized for acute injuries resulted in lower PTSD symptom burden and alcohol abuse/dependence.
Bipolar Disorder
The 2021 SPIRIT study examined CoCM for patients with bipolar disorder and/or PTSD and compared CoCM to care provided by both a psychologist and a psychiatrist. Researchers found that CoCM was equally effective as care delivered by a specialist team. This finding is impressive but it’s important to keep in mind that patients in the CoCM arm of the study had a one-time diagnostic interview with a psychiatric provider, and the psychiatric consultant discussed their case much more frequently than standard CoCM protocols for treating depression or anxiety. This suggests potential adjustments in resource allocation, for example, reducing a Behavioral Health Care Manager's (BHCM) caseload size.
Dementia
As the population ages and life expectancy increases, there is growing evidence that CoCM can be effective with dementia. A review published in 2020 showed that patients being treated with CoCM had fewer behavioral symptoms of dementia, improved functioning and quality of life, lower utilization of acute medical services, and decreased caregiver burden when compared with usual care.
Substance Use Disorders
The landmark SUMMIT research trial examined a CoCM approach to treating alcohol and opioid use disorders in primary care. Patients receiving CoCM were significantly more likely than patients in usual care to access treatment and abstain from alcohol and drugs. The American Psychiatric Association summarizes some of the important considerations when treating substance use disorders with CoCM.
Tailoring CoCM program to meet diverse needs
Collaborative Care can be used to treat a wide range of behavioral health conditions in primary care and other medical settings. Its proven effectiveness across diverse conditions underscores its pivotal role in enhancing patient outcomes and reducing healthcare disparities.
As the evidence base evolves, many practices are now developing caseloads capable of treating patients with a wide range of mental health conditions. When implementing a CoCM program, it’s crucial to think about the specific conditions your team will address. This should guide your hiring and training decisions. For example, if your program will focus on substance abuse, consider bringing on a Psychiatric Consultant who has experience with addictions. Or, providing training to the BHCM on brief behavioral interventions proven effective with diverse behavioral health conditions, like behavioral activation (which was used in the SPIRIT study), could also be beneficial. Remember, many of these conditions come with a range of physical and behavioral health co-morbidities. So, when determining the caseload size for the BHCM, make sure to account for this complexity.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|
|
|