keyword: collaborative care
Registry Innovations in Collaborative Care
Treating Substance Use in Collaborative Care
Advocacy for Collaborative Care
Comparing Collaborative Care to Usual Care
Introduction:
Compared with usual care, Collaborative Care has been shown to improve the effectiveness of depression treatment and lower total healthcare costs. This handout outlines those differences using data from the IMPACT trial.
A printable PDF is available for download; however, please note that this document may not conform to the WCAG-2 accessibility standards.
Comparing Collaborative Care to Usual Care
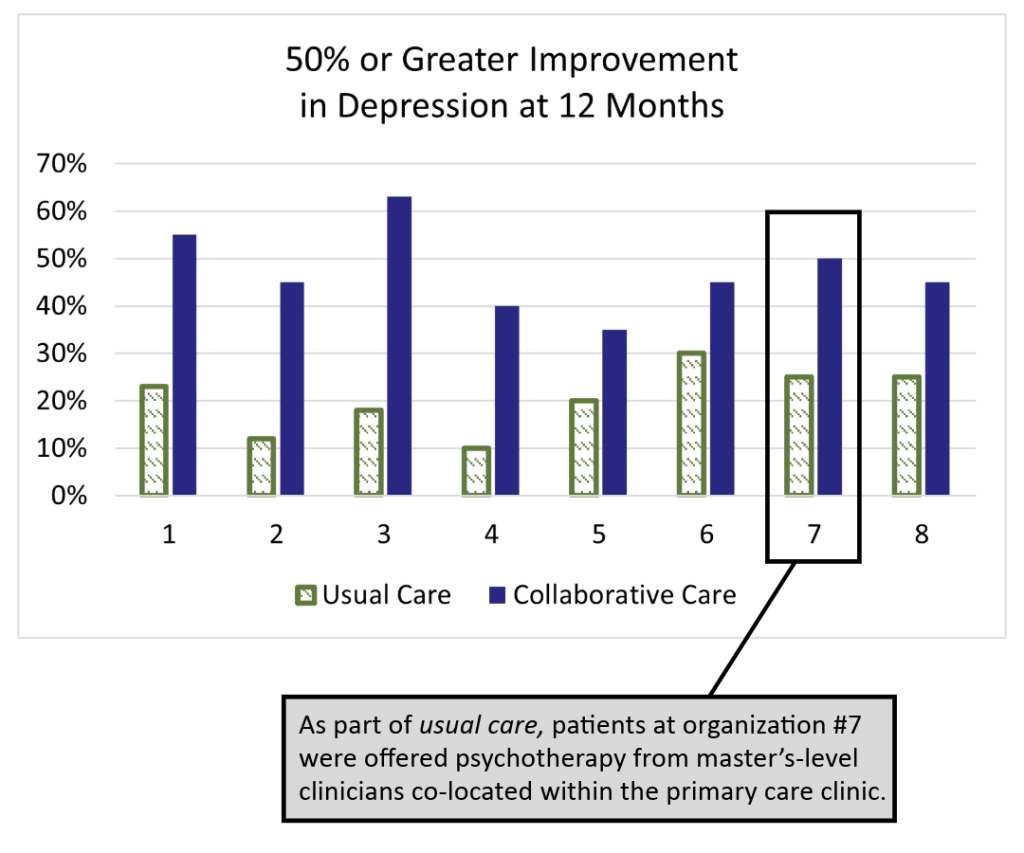
The IMPACT (Improving Mood: Providing Access to Collaborative Treatment) trial focused on depressed, older adults. Half were randomly assigned to receive the depression treatment usually offered by participating clinics, and half were randomly assigned to receive collaborative care. Collaborative care more than doubled the effectiveness of depression treatment and reduced total healthcare costs at the same time (JAMA, 2002).
Usual Care
50% of study patients used antidepressants at the time of enrollment, but were still significantly depressed.
70% of usual care patients received medication therapy from their PCP and/or a referral to specialty behavioral health.
Only 20% of patients showed significant improvements after one year, which matches national data for depression treatment in primary care.
Collaborative Care
On average, twice as many patients significantly improved. The difference was statistically significant in all eight healthcare settings. Why?
- Patient-Centered Team Care
- Population-Based Care
- Measurement-Based Treatment to Target
- Evidence-Based Care
- Accountable Care
Why Practice Collaborative Care?
Introduction:
This resource outlines the benefits of Collaborative Care and is designed to be shared with PCPs, stakeholders, and others looking to implement CoCM.
For a printable version, download the resource below. A printable PDF is available for download; however, please note that this document may not conform to the WCAG-2 accessibility standards.
Why Practice Collaborative Care?
Collaborative care (CoCM) is beneficial to primary care providers (PCPs) and their patients because it offers better
medical care, access to psychiatry experts, helps with challenging patient cases, and team collaboration.

Established Evidence Base
- CoCM has a robust evidence base of over 80 randomized controlled trials and has been shown to be the best approach to treating depression in many populations and settings.
- CoCM has a strong and expanding evidence base for its use with diverse behavioral health diagnoses such as anxiety, posttraumatic stress disorder, chronic pain, and dementia.

Better Medical Outcomes
- CoCM is linked to better medical outcomes for patients with diabetes, cardiovascular disease, cancer, and chronic arthritis.
- CoCM is recommended as a primary prevention strategy for cardiovascular events in patients without preexisting heart disease (Psychosomatic Medicine, 2014).

Help with Challenging Patient Cases
- Many challenging cases likely have patients with untreated or undertreated behavioral health conditions. Behavioral health providers do the follow-up and intervention tasks that a busy PCP doesn’t have time to do, but make a big difference for patients.
- PCPs are generally more satisfied working within an integrated behavioral health care program than within usual care (Family Community Health, 2015).

Faster Improvement
- A 2016 retrospective study at Mayo Clinic found that the time to depression remission was 86 days in a CoCM program while in usual care it was 614 days.
- Analysis of a large CoCM implementation found that early, intense intervention by the behavioral health provider was key to early improvement in patients with depression symptoms (Psychiatric Services, 2015).
It Takes a Team
- CoCM uses an enhanced care team to provide a population based, treat-to-target approach to care. Through shared care planning, the team makes proactive changes in treatment to make sure that no patients fall through the cracks.
- Only 30-50% of patients have a full response to the first treatment. That means 50-70% of patients need at least one treatment adjustment. Additional experts can help.
Evidence Base for Collaborative Care
A substantial body of evidence for Collaborative Care has emerged since its development at the University of Washington in the 1990s. Beginning with the seminal IMPACT Trial published in 2002, more than ninety randomized controlled trials and several meta-analyses show that Collaborative Care (CoCM) is more effective than usual care for patients with depression, anxiety, and other behavioral health conditions.
CoCM is also shown to be highly effective in treating co-morbid mental health and physical conditions such as cancer, diabetes, and HIV. The document summarizes several selected research, review, and practice-based articles that demonstrate Collaborative Care significantly improves patient lives.
Tips for Discussing Trauma During an Initial Assessment
Introduction
Trauma can increase the risk of health, social, and emotional problems. Despite the high prevalence of patients with a past history of trauma, few clinics or Collaborative Care teams have a protocol for addressing it. These three tips can help clinicians safely and effectively discuss the trauma history of their patients during their initial assessment.
A printable PDF is available for download; however, please note that this document may not conform to the WCAG-2 accessibility standards.
Discussing Past Trauma with Patients During an Initial Assessment
Many patients with depression have experienced trauma in their lives. Discussing the past traumas in a patient’s life can be tricky due to the risk of re-traumatization or re-triggering the symptoms related to Post-Traumatic Stress Disorder (PTSD). It is also common for the patient to dissociate as a defense mechanism to avoid their past trauma. We have compiled a few tips to help clinicians talk with their patients about past trauma and safely learn their stories during an Initial Assessment.
This is only the beginning of a very complex subject. For more information about caring for patients with trauma history, please read “TIP 57: Trauma-Informed Care in Behavioral Health Services” by SAMHSA.
Tip 1
To prevent re-traumatizing or re-triggering PTSD symptoms, encourage the patient to respond with short, concise descriptions of the trauma.
- Ask for a 2-3 sentence or <25 word description to get a general sense of the trauma.
- Be directive and feel free to stop the discussion if you see the patient is having trouble containing their emotions.
- Normalize the extreme difficulty patients often have when re-telling their stories.
Tip 2
Don’t start with a checklist! Patients often have post-injury concerns and interpret trauma uniquely.
- Encourage the patient to tell their story in their own words.
- Ask open-ended questions.
- Remember, you don’t need all the details to make the diagnosis or treat depression!
Tip 3
If you notice the patient dissociate, work with them to help them get grounded and then educate them on dissociation.
- A way to help ground the patient is to direct them to engage in their immediate environment.
- Once they are grounded, educate them on dissociation.
Tips adapted from: Stephens, K., & Bentham, W. (2010, June 17). PTSD in Primary Care. Mental Health Integration Program (MHIP) Webinar.
Medicare Payment for Behavioral Health Integration
An article published in the New England Journal of Medicine discusses the Center for Medicare and Medicaid Sevices’ payment codes for behavioral health integration.
Quick Guide on Behavioral Health Integration Services
The Centers for Medicare & Medicaid Services (CMS) annually updates Medicare guidelines and payments for services provided by medical treating providers for patients participating in a Collaborative Care program or receiving other behavioral health integration services. This handout summarizes the Medicare codes and guidelines.
The payment structure may be used to treat patients with any behavioral health condition that is being treated by the billing practitioner, including substance use disorders.