A printable flyer offering an overview of the AIMS Center’s work to share with your networks.
Implementation Tool: Getting Started
Checklist of Collaborative Care Principles and Components
Core principles and components of effective integrated behavioral health care developed in consultation with national experts and support from the John A. Hartford Foundation, the Robert Wood Johnson Foundation, the Agency for Healthcare Research and Quality, and the California HealthCare Foundation.
Comparing Collaborative Care to Usual Care
Introduction:
Compared with usual care, Collaborative Care has been shown to improve the effectiveness of depression treatment and lower total healthcare costs. This handout outlines those differences using data from the IMPACT trial.
A printable PDF is available for download; however, please note that this document may not conform to the WCAG-2 accessibility standards.
Comparing Collaborative Care to Usual Care
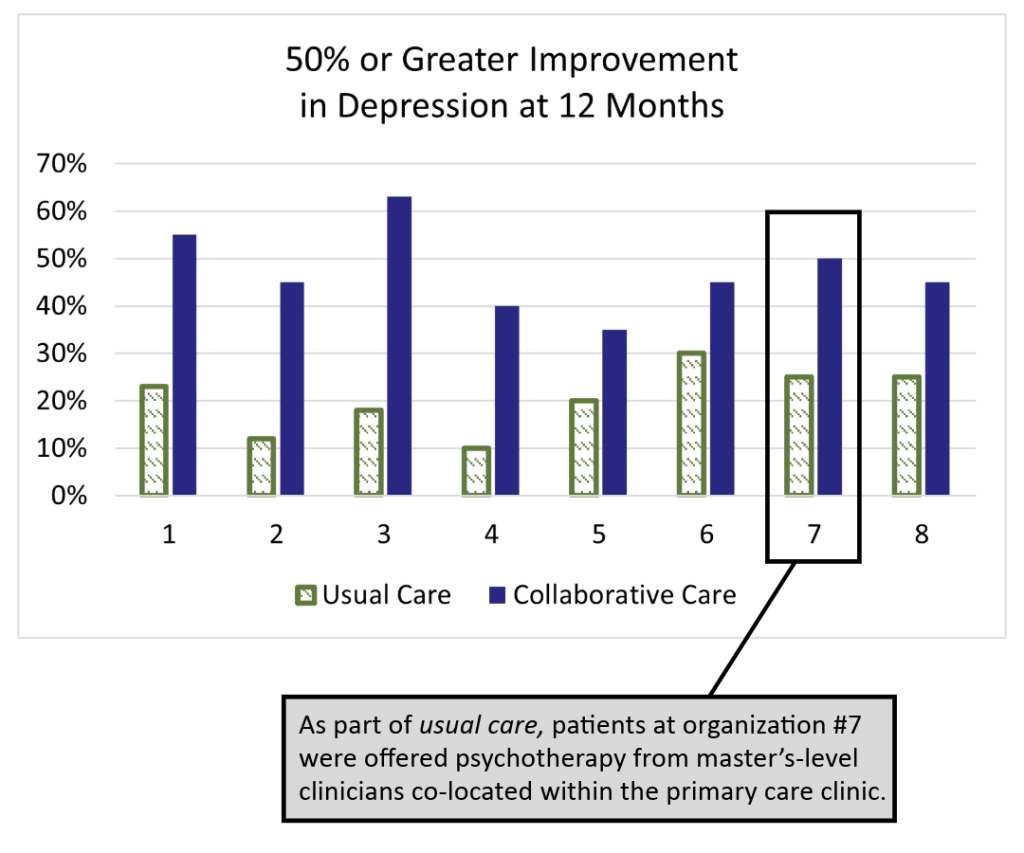
The IMPACT (Improving Mood: Providing Access to Collaborative Treatment) trial focused on depressed, older adults. Half were randomly assigned to receive the depression treatment usually offered by participating clinics, and half were randomly assigned to receive collaborative care. Collaborative care more than doubled the effectiveness of depression treatment and reduced total healthcare costs at the same time (JAMA, 2002).
Usual Care
50% of study patients used antidepressants at the time of enrollment, but were still significantly depressed.
70% of usual care patients received medication therapy from their PCP and/or a referral to specialty behavioral health.
Only 20% of patients showed significant improvements after one year, which matches national data for depression treatment in primary care.
Collaborative Care
On average, twice as many patients significantly improved. The difference was statistically significant in all eight healthcare settings. Why?
- Patient-Centered Team Care
- Population-Based Care
- Measurement-Based Treatment to Target
- Evidence-Based Care
- Accountable Care
Why Practice Collaborative Care?
Introduction:
This resource outlines the benefits of Collaborative Care and is designed to be shared with PCPs, stakeholders, and others looking to implement CoCM.
For a printable version, download the resource below. A printable PDF is available for download; however, please note that this document may not conform to the WCAG-2 accessibility standards.
Why Practice Collaborative Care?
Collaborative care (CoCM) is beneficial to primary care providers (PCPs) and their patients because it offers better
medical care, access to psychiatry experts, helps with challenging patient cases, and team collaboration.

Established Evidence Base
- CoCM has a robust evidence base of over 80 randomized controlled trials and has been shown to be the best approach to treating depression in many populations and settings.
- CoCM has a strong and expanding evidence base for its use with diverse behavioral health diagnoses such as anxiety, posttraumatic stress disorder, chronic pain, and dementia.

Better Medical Outcomes
- CoCM is linked to better medical outcomes for patients with diabetes, cardiovascular disease, cancer, and chronic arthritis.
- CoCM is recommended as a primary prevention strategy for cardiovascular events in patients without preexisting heart disease (Psychosomatic Medicine, 2014).

Help with Challenging Patient Cases
- Many challenging cases likely have patients with untreated or undertreated behavioral health conditions. Behavioral health providers do the follow-up and intervention tasks that a busy PCP doesn’t have time to do, but make a big difference for patients.
- PCPs are generally more satisfied working within an integrated behavioral health care program than within usual care (Family Community Health, 2015).

Faster Improvement
- A 2016 retrospective study at Mayo Clinic found that the time to depression remission was 86 days in a CoCM program while in usual care it was 614 days.
- Analysis of a large CoCM implementation found that early, intense intervention by the behavioral health provider was key to early improvement in patients with depression symptoms (Psychiatric Services, 2015).
It Takes a Team
- CoCM uses an enhanced care team to provide a population based, treat-to-target approach to care. Through shared care planning, the team makes proactive changes in treatment to make sure that no patients fall through the cracks.
- Only 30-50% of patients have a full response to the first treatment. That means 50-70% of patients need at least one treatment adjustment. Additional experts can help.
Evidence Base for Collaborative Care
A substantial body of evidence for Collaborative Care has emerged since its development at the University of Washington in the 1990s. Beginning with the seminal IMPACT Trial published in 2002, more than ninety randomized controlled trials and several meta-analyses show that Collaborative Care (CoCM) is more effective than usual care for patients with depression, anxiety, and other behavioral health conditions.
CoCM is also shown to be highly effective in treating co-morbid mental health and physical conditions such as cancer, diabetes, and HIV. The document summarizes several selected research, review, and practice-based articles that demonstrate Collaborative Care significantly improves patient lives.
Time to Remission for Depression with Collaborative Care Management (CCM) in Primary Care
Researchers from the Mayo Clinic conducted a retrospective study that found that collaborative care management improved the time to remission as well as shortened the duration of persistent depressive symptoms in patients diagnosed with depression.
Integrated Care: Creating Effective Mental and Primary Health Care Teams
Integrated Care: Creating Effective Mental Health and Primary Health Care Teams provides the first comprehensive guide for teams to integrate effective mental health care into primary care clinics. Edited by a team of UW Medicine mental health experts, it includes practical information, skills, and clinical approaches needed to implement Collaborative Care, an evidence-based model of integrated care developed at the University of Washington. Importantly, it provides a common resource and framework for all members of the care team including care managers, psychiatrists, primary care providers, and administrators. Editors include UW psychiatrists Anna Ratzliff, MD, PhD, Jurgen Unutzer, MD, PhD, MA, and the late Wayne Katon, MD, as well as UW psychologist Kari Stephens, PhD.
Find resources for implementation within the free Integrated Care Online Appendix. These include a CoCM readiness checklist, BHCM documentation templates with examples, job descriptions, links to screening and symptom monitoring tools, and more.
Email uwaims@uw.edu with specific questions.
Please note:
The Integrated Care Online Appendix can be found on the publisher’s website under ‘downloads’ at the bottom of the page.