Introduction
Primary care clinics have a responsibility to provide effective and efficient suicide safe care that is accessible to all patients and staff. Developing a thoughtful and clear protocol and workflow for responding to suicidality in your primary care setting will empower staff to know how to act as well as help keep patients and staff safe.
The resource below contains information about screening and identification, conducting risk assessments, response and follow-up to suicide risk, as well as several additional resources. This information is intended to guide primary care clinics to refine existing protocol(s) for responding to patients presenting with suicidality or violent behavior in a primary care clinic.
A printable PDF is available for download; however, please note that this document may not conform to the WCAG-2 accessibility standards.
Developing Protocols for Suicide Prevention in Primary Care
Primary care clinics have a responsibility to provide effective and efficient suicide safe care that is accessible to all patients and staff. Developing a thoughtful and clear protocol and workflow for responding to suicidality in your primary care setting will empower staff to know how to help keep patients safe. This information is intended to guide primary care clinics to refine existing protocol(s) for responding to patients presenting with suicidality in a primary care clinic.
Principles
All clinic staff are informed and supported
One-page workflows for responding to suicidal ideation should be easily accessible to all staff (not just the behavioral health staff or the clinic manager). These workflows should clearly outline when and how to respond, who to engage, and list internal and external resources. The 988 Suicide and Crisis Lifeline or other relevant emergency/crisis numbers are easily available. And staff are informed on how to contact the crisis response teams if available in your setting.
Collaboratively develop safety plans
A safety plan provides guidance and resources for the patient to reduce their risk of suicidal behavior. This is a collaborative document that includes holistic assessment paired with individualized intervention, as opposed to a safety contract, which is an agreement not to self-harm. There is no evidence that contracting for safety with a patient is effective at reducing suicides. In addition, contracts have no legal meaning and may give a false sense of security to a provider.
Take risk seriously
Primary care clinics should be screening patients to identify those at risk of suicide. Appropriate risk assessment and intervention should be completed for every patient identified with risk of suicide, every time.
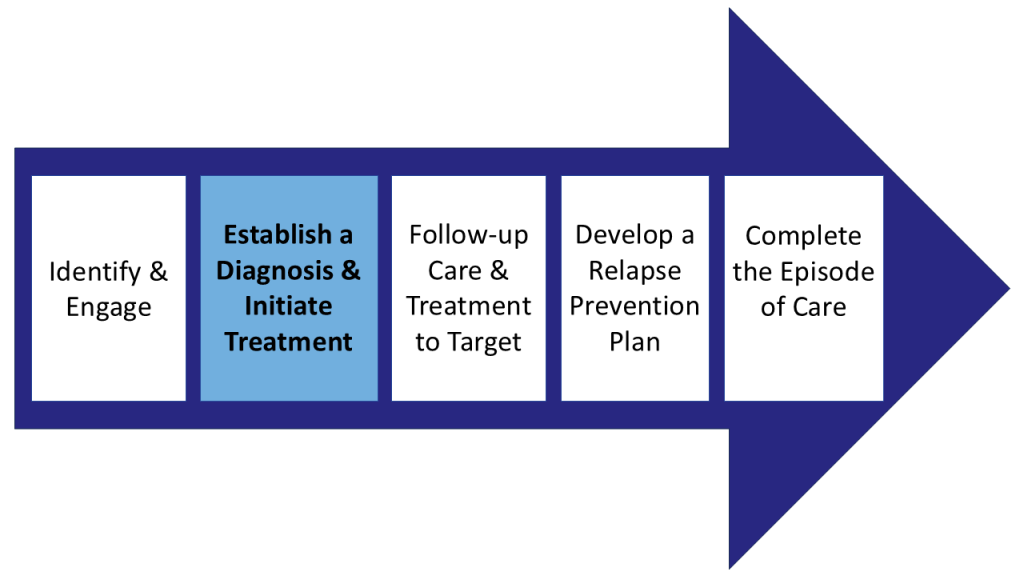
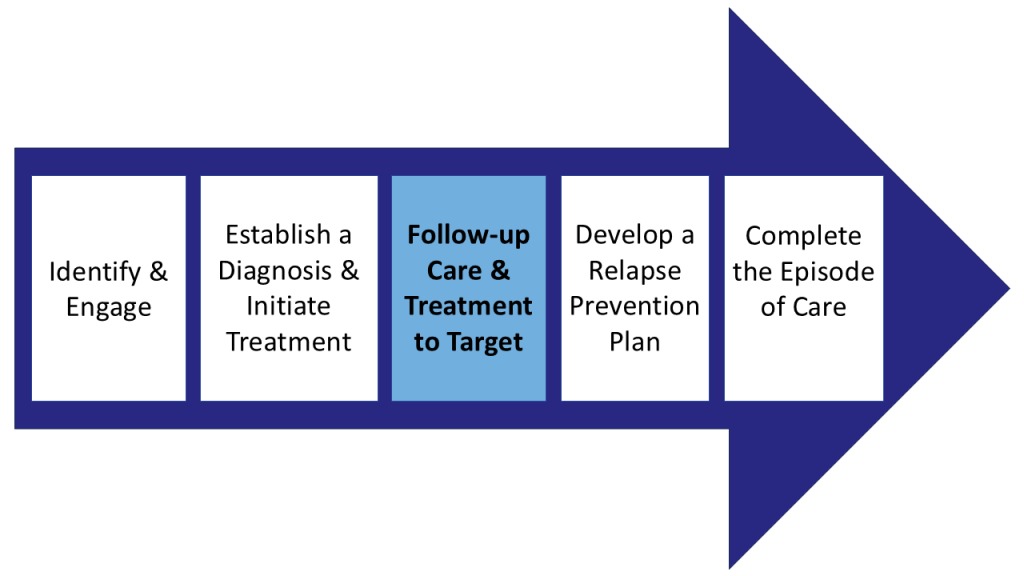
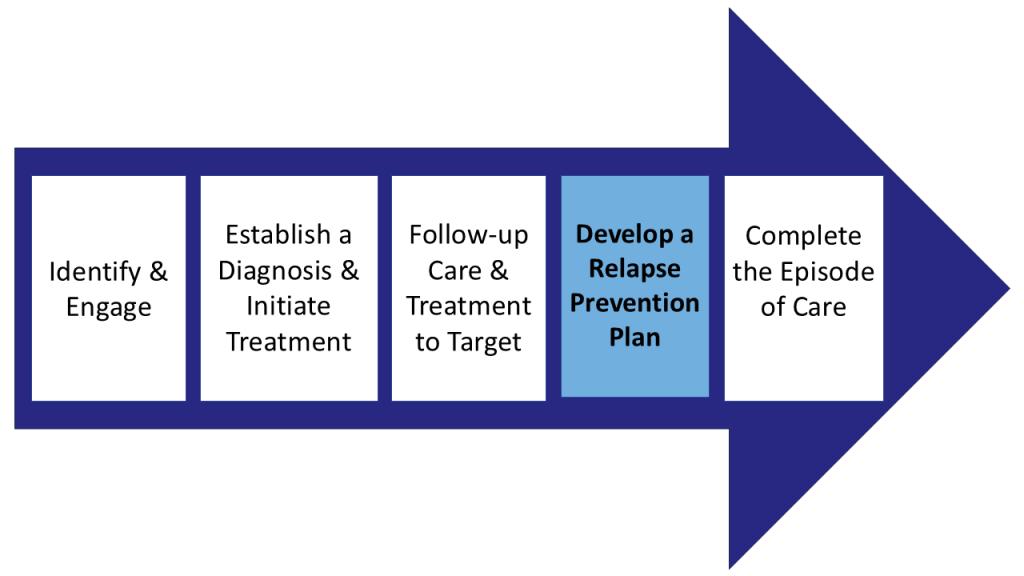
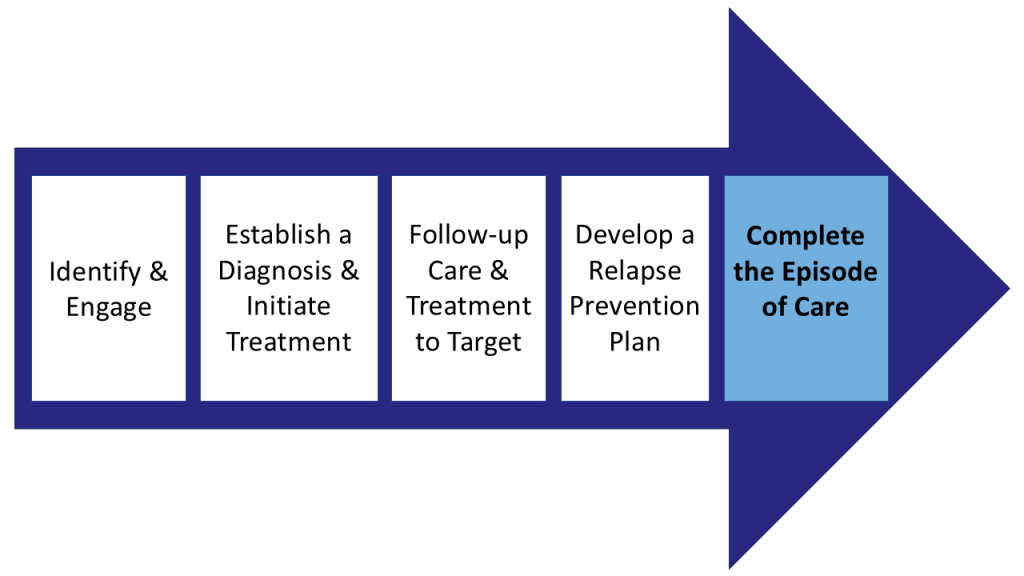
Suicide Prevention Protocol Elements
The below sections provide descriptions of the key suicide prevention protocol elements, as follows:
- Screening and identification of suicide risk
- Asking about and assessing suicide risk level
- Responding to suicide risk level
- Follow up & next steps in care
1. Screening and identification of patients at risk of suicide
Any patient presenting for mental health or substance use treatment should be screened for thoughts of suicide with a validated screening tool. The PHQ9 question #9 is one example. It reads, “Have you been having thoughts that you would be better off dead or thoughts of hurting yourself in some way?”. When a patient scores positive for suicide risk, further information should be gathered.
Resource:
PHQ-9 Depression Scale
2. Ask about and assess suicide risk level to determine next steps
To determine suicide risk level, a trained staff person should administer a validated screening tool like the Columbia-Suicide Severity Rating Scale (C-SSRS), Ask Suicide-Screening Questions (ASQ) and/or the Suicide Assessment Five-Step Evaluation and Triage (Safe-T). Providers should be trained to communicate with patients who are suicidal in a calm, curious, and caring manner. Validated tools when combined with clinical judgement can help determine levels of risk and aid in making clinical decisions about care.
In general, suicide risk level can be grouped into two categories:
Non-Acute Risk
Imminent risk of completing suicide is not identified; indicates the patient can safely continue treatment in primary care with appropriate intervention.
Acute Risk
Imminent risk of completing suicide is identified; indicates patient should be under safe observation until a crisis response team completes an evaluation or patient is taken to an Emergency Department for potential hospitalization.
Levels of risk can be classified differently depending on the validated tool used. Some tools, like the C-SSRS or SAFE-T assign “high”, “moderate” or “low” values influenced by modifiable risk factors and protective factors. Classifications like these support interventions that are responsive to patient risk level.
Resources:
3. Responding to suicide risk level
Non-Acute Risk Interventions: If risk is non-acute, the next step is to develop a collaborative safety plan. This is an important clinical component of treating a patient in an outpatient setting. Even when a patient is experiencing passive suicidal ideation, a safety plan should be done because suicide risk is not fixed and can change over time. Safety planning should address risk factors that can be modified, including limiting access to lethal means.
Acute Risk Interventions: If risk is acute, the provider should have a direct conversation about next steps for maintaining the patient’s safety. A clinic staff member should remain with the patient until the patient is evaluated by a crisis response team or in safe transport to an Emergency Department. Clinic staff should be trained on how to coordinate and provide relevant chart notes for the referral. A plan should be in place for appropriate action if a patient refuses care or leaves the clinic against medical advice (AMA). This may include contacting a crisis response team or the police.
Resource(s):
4. Follow up & next steps in care
The clinic should have a clear process to follow up with patients who have presented with suicidal risk. This includes clear guidelines on how to regularly track, follow up on and review safety plans with patients. Staff should be trained in where to find completed plans in the EHR.
For patients who receive further evaluation by a crisis response team or Emergency Department, the primary care clinic should have a plan for coordinating care, including who is responsible for documenting and communicating evaluation outcomes and patient care plan with the team.
The clinic should offer support and follow up to staff who may be impacted by a patient treated for suicide risk or who dies by suicide.
Resource(s):