Introduction:
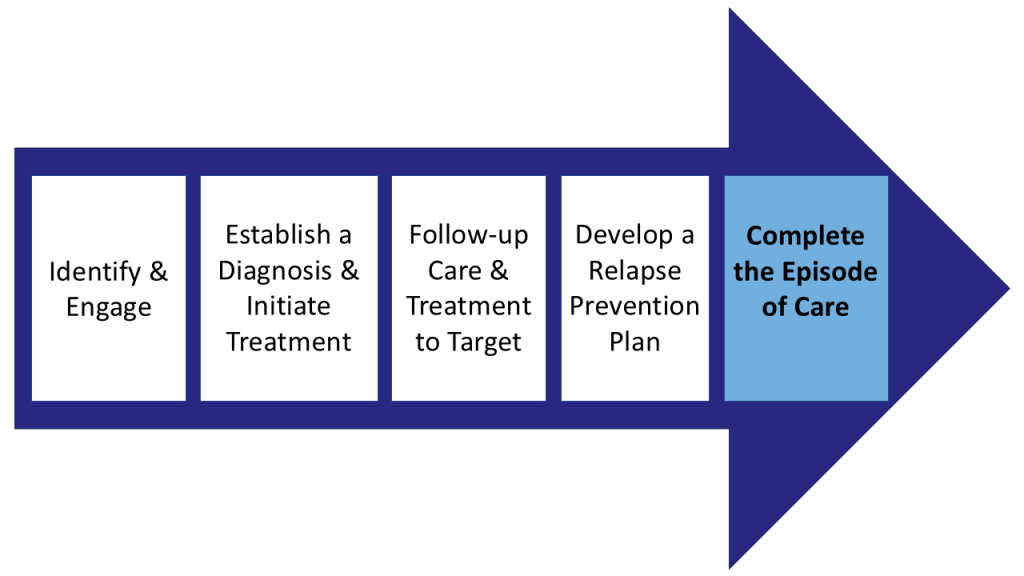
Successful Collaborative Care (CoCM) programs have a defined, detailed workflow that maps the patient journey from screening to the end of an episode of care. These workflows detail the five phases of an episode of CoCM. Each phase has a unique set of tasks tailored to the resources available at the site. These workflows should be accessible to those who use them and describe steps with sufficient detail.
A printable PDF is available for download; however, please note that this document may not conform to the WCAG-2 accessibility standards.
Creating Collaborative Care Workflows
Creating workflows is an iterative, team process. Much like creating a shared vision, this process includes a series of team discussions facilitated by the Clinic Implementation Team (CIT) lead.
Your workflows will be a detailed version of the 5 phases of an episode of Collaborative Care (CoCM). Each phase will have a unique set of tasks, tailored to the resources available at your site. Please see the full CoCM Workflow Development Guide for more details.
We recommend the team create a process map or visual workflow for each of the five phases of an episode of CoCM. Make sure the workflows describe the steps in sufficient detail and are accessible to those who need it.

Phase 1: Identify & Engage
- Behavioral health screening &/or population health report, &/or PCP assessment to identify patients
- Introduce CoCM
- Consent patients to participate in CoCM
- Connect patients to the Behavioral Health Care Manager (BHCM)
- When suicidality is identified through the behavioral health screening process, it is important to have a protocol in place
Phase 2: Establish a Diagnosis & Initiate Treatment
- BHCM completes Initial Assessment. Enroll the patient in CoCM and add them to the registry.
- Generate a provisional diagnosis as a CoCM team (PCP, Psychiatric Consultant, BHCM)
- Explore treatment options with the patient (brief evidence- based behavioral interventions, medications, or both)
- Communicate treatment plans with the CoCM team
Phase 3: Follow-up Care & Treatment to Target
- Proactive and continuous outreach from BHCM to the patient
- Track patient progress in a registry
- Use a registry to identify patients who need to be discussed at the Systematic Caseload Review (SCR)
- Hold SCR weekly sessions between the BHCM and the Psychiatric Consultant
- Consider the frequency for administration of symptom monitoring tools (e.g. PHQ-9, GAD-7, PCL-5, etc.)
Phase 4: Develop a Relapse Prevention Plan
- Determine criteria to begin a Relapse Prevention Plan (RPP)
- BHCM initiates RPP with the patient
- Determine how often to connect with the patient during the monitoring phase
- Consider how RPP will be documented, stored, and communicated with the patient, as well as the CoCM team
Phase 5: Complete the Episode of Care
- Develop a workflow for each possible completion pathway:
- Transition improved patients back to their PCP for follow-up care, with the option to return for another episode of CoCM if symptoms worsen
- Referral to specialty behavioral health for patients with severe symptoms that are not improving in CoCM
- Discontinue the episode for patients who cannot be reached
Need help building your workflow?
- See Step 2: Plan for Clinical Practice Change of our Implementation Guide
- Get expert assistance from the AIMS Center